Case Capsule
- 50 year old man presented with complaints of headache and behavioural change of 3 months duration in July 2011.
- Associated with gait disturbances of 1 month duration
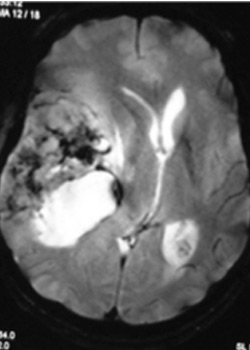
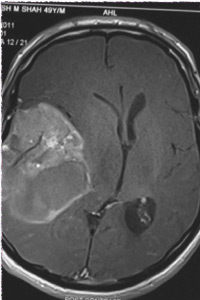
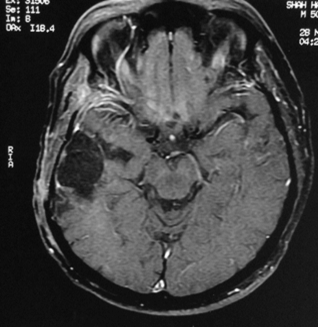
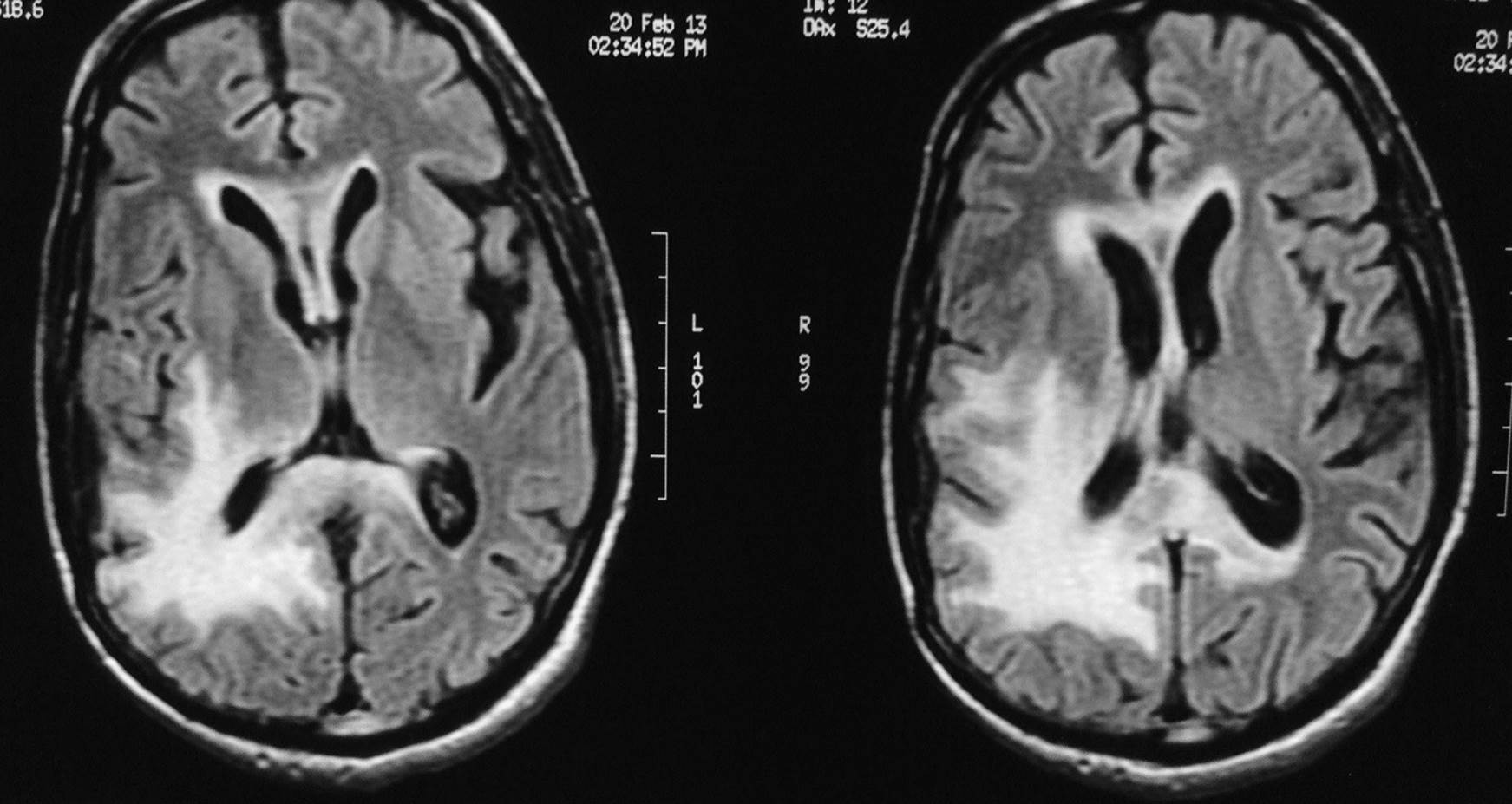
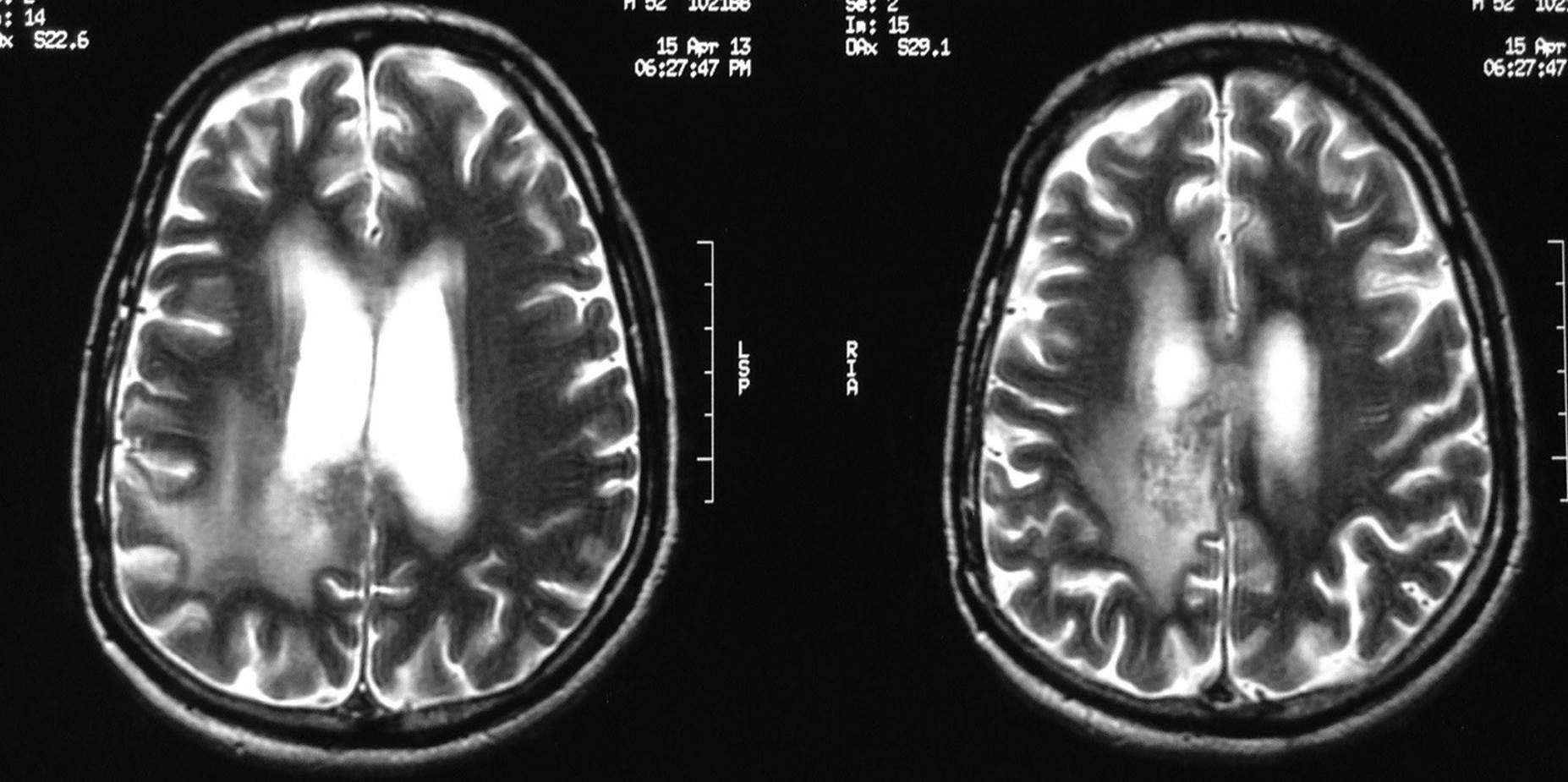
- Pre-operative MRI (02.08.2011) showed a large complex solid cystic enhancing intraaxial mass lesion in the right temporo-parietal and frontal region
T2 FLAIR images
He underwent radical excision by right temporo-parietal craniotomy and excision on 05.08.2011

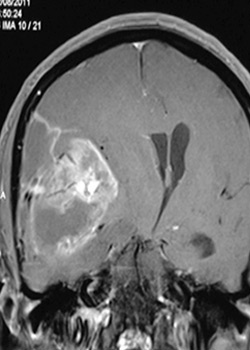
- Post operative MRI on 18.08.2011 shows good exicision of the mass
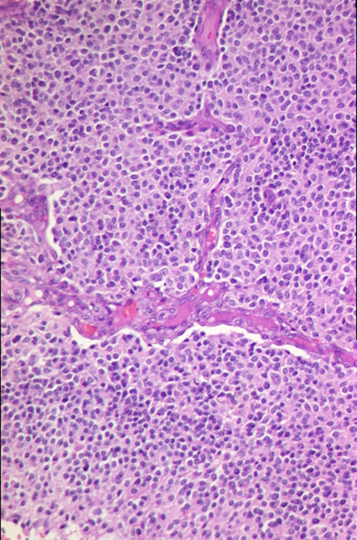
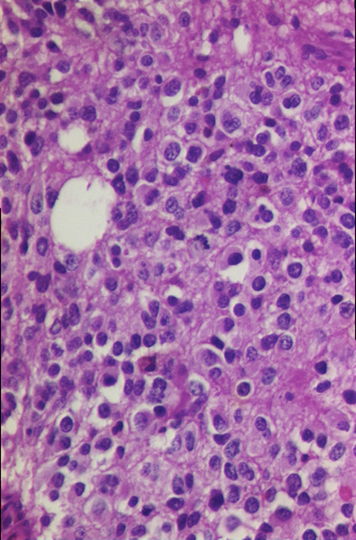
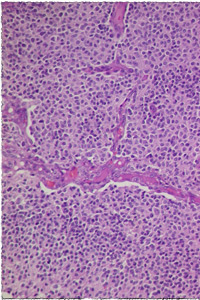
- High grade glial tumour with oligodendroglial component
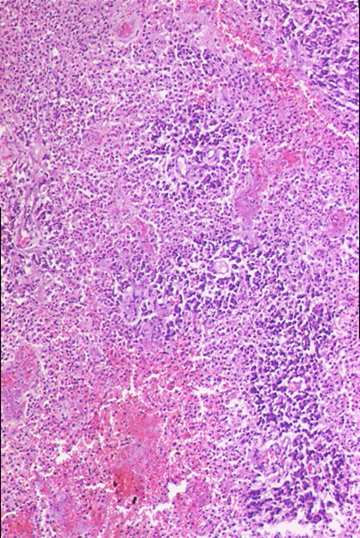
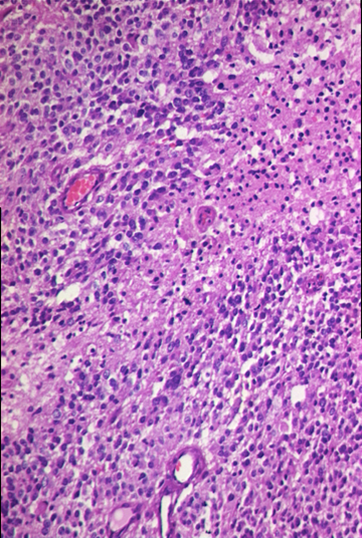
- Significant large confluent areas of necrosis
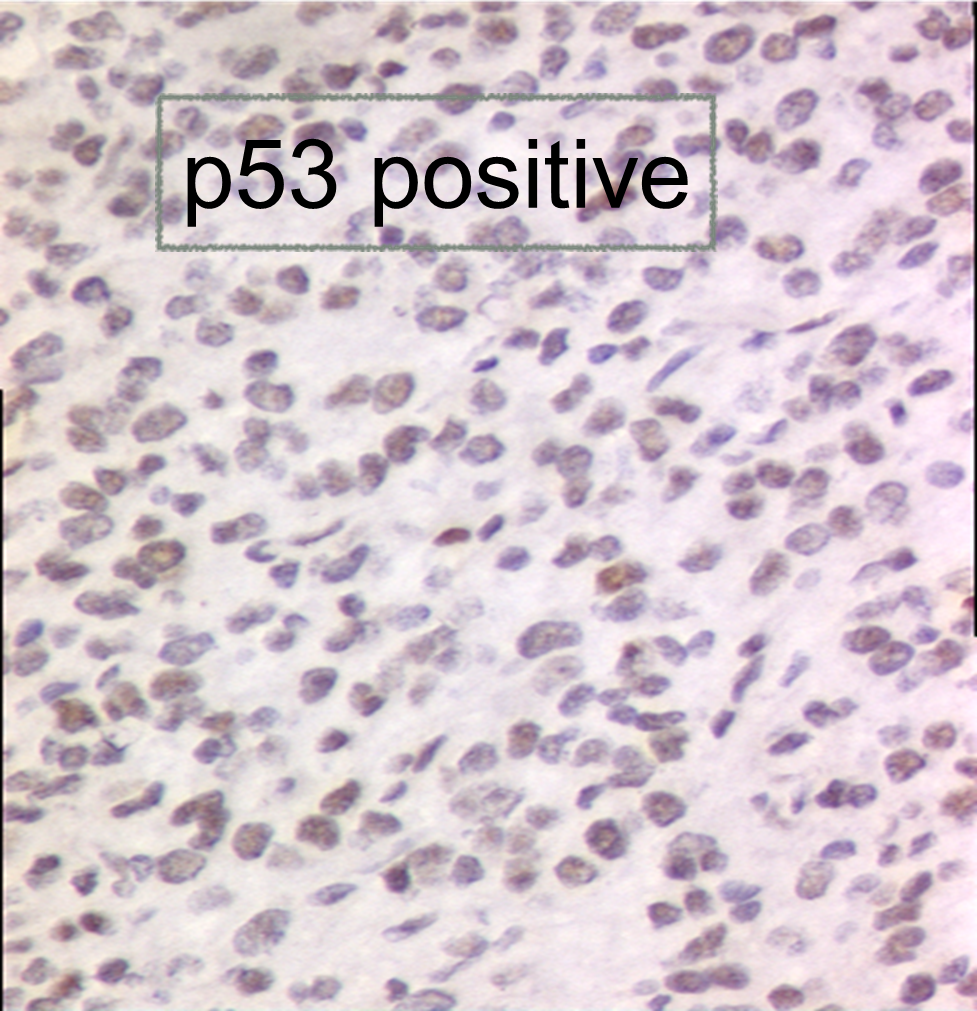
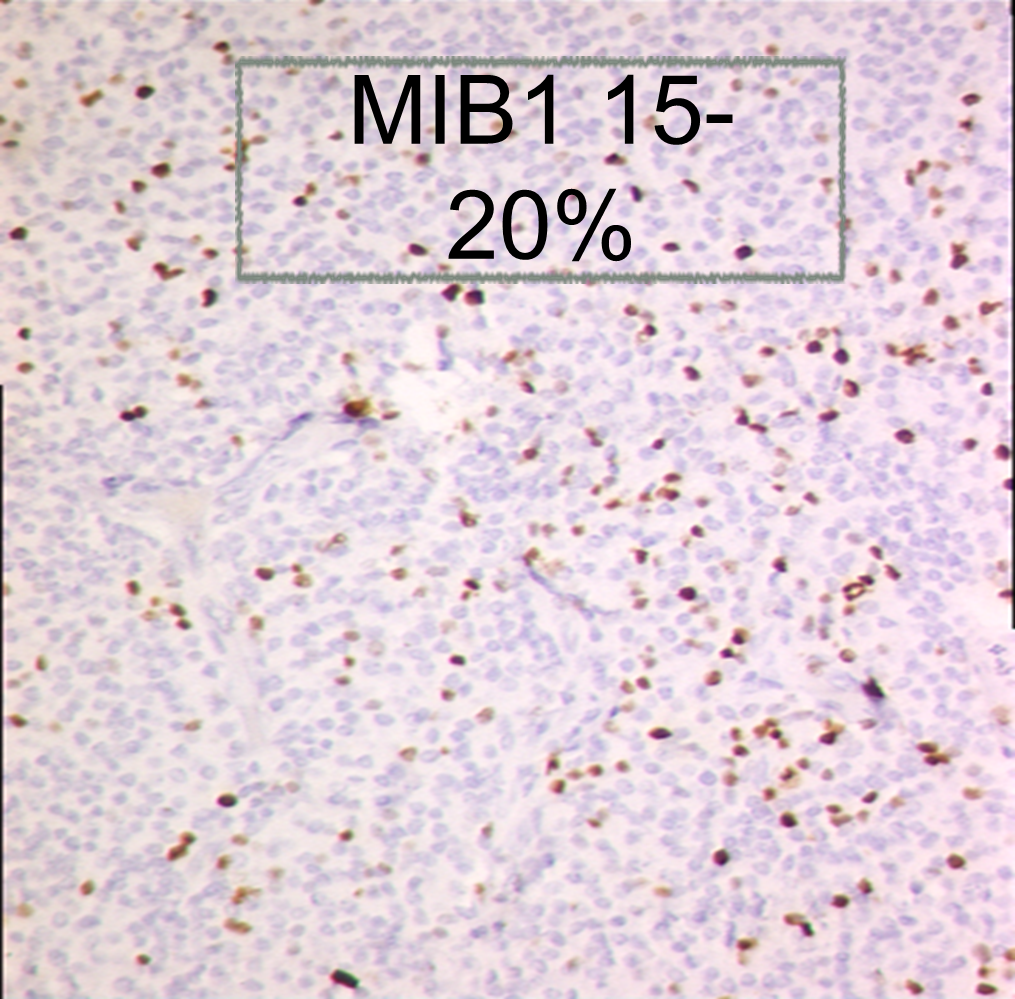
- GBM with oligodendroglial component (GBM-O) versus anaplastic oligodendroglioma were proposed as differentials. Former was favoured
- Plan : Adjuvant concurrent chemoradiation.
- He concluded focal conformal radiotherapy (59.4Gy/33#) along with Cap Temozolomide (75mg/sq. metre) on 02.11.2011.
- Tolerated the treatment well.
1st follow up post chemoradiation MRI scan on 28.11.2011
- Patient clinically well without any deficits
T2 Images
MRI scan 28.11.2011
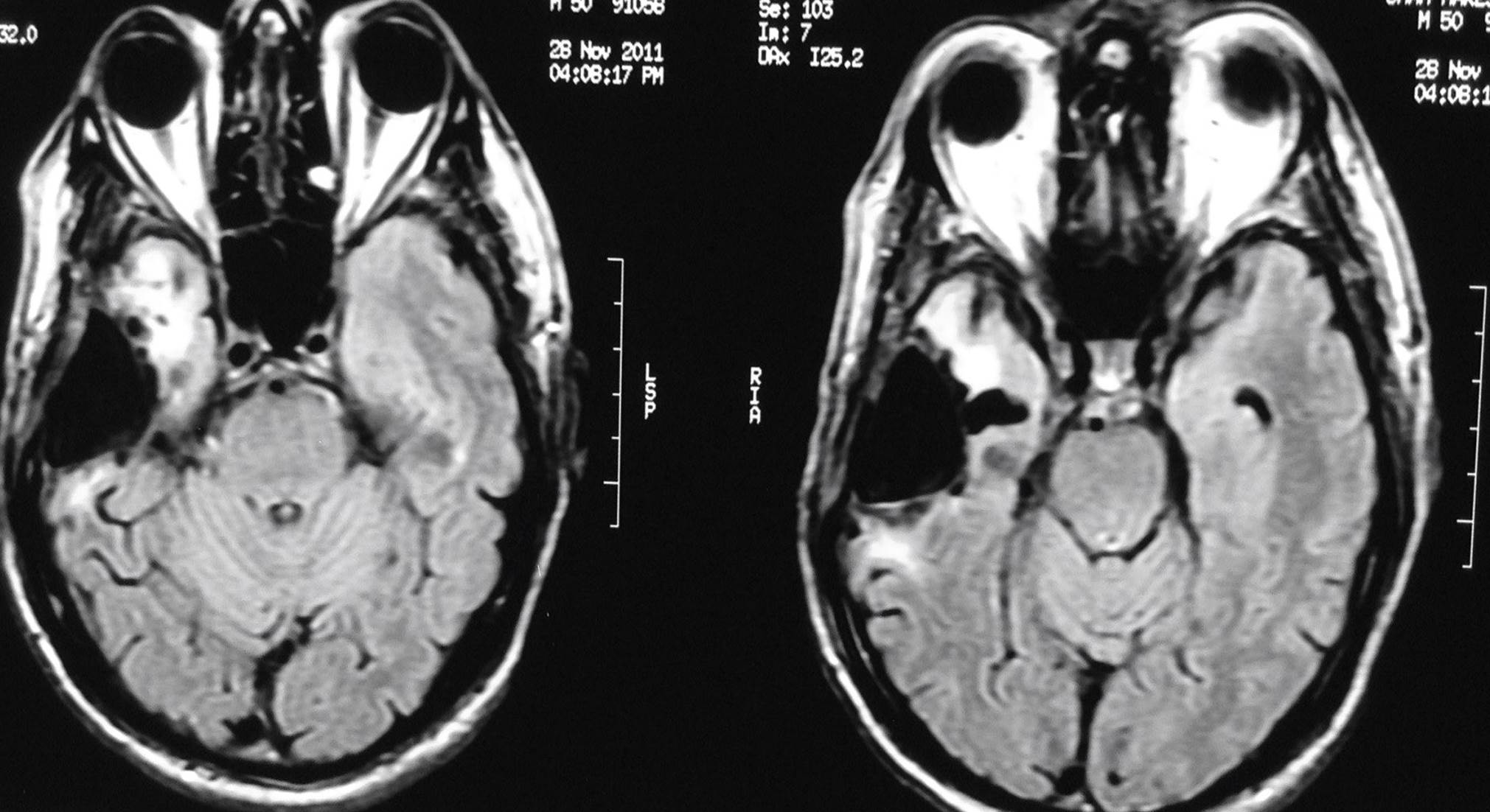
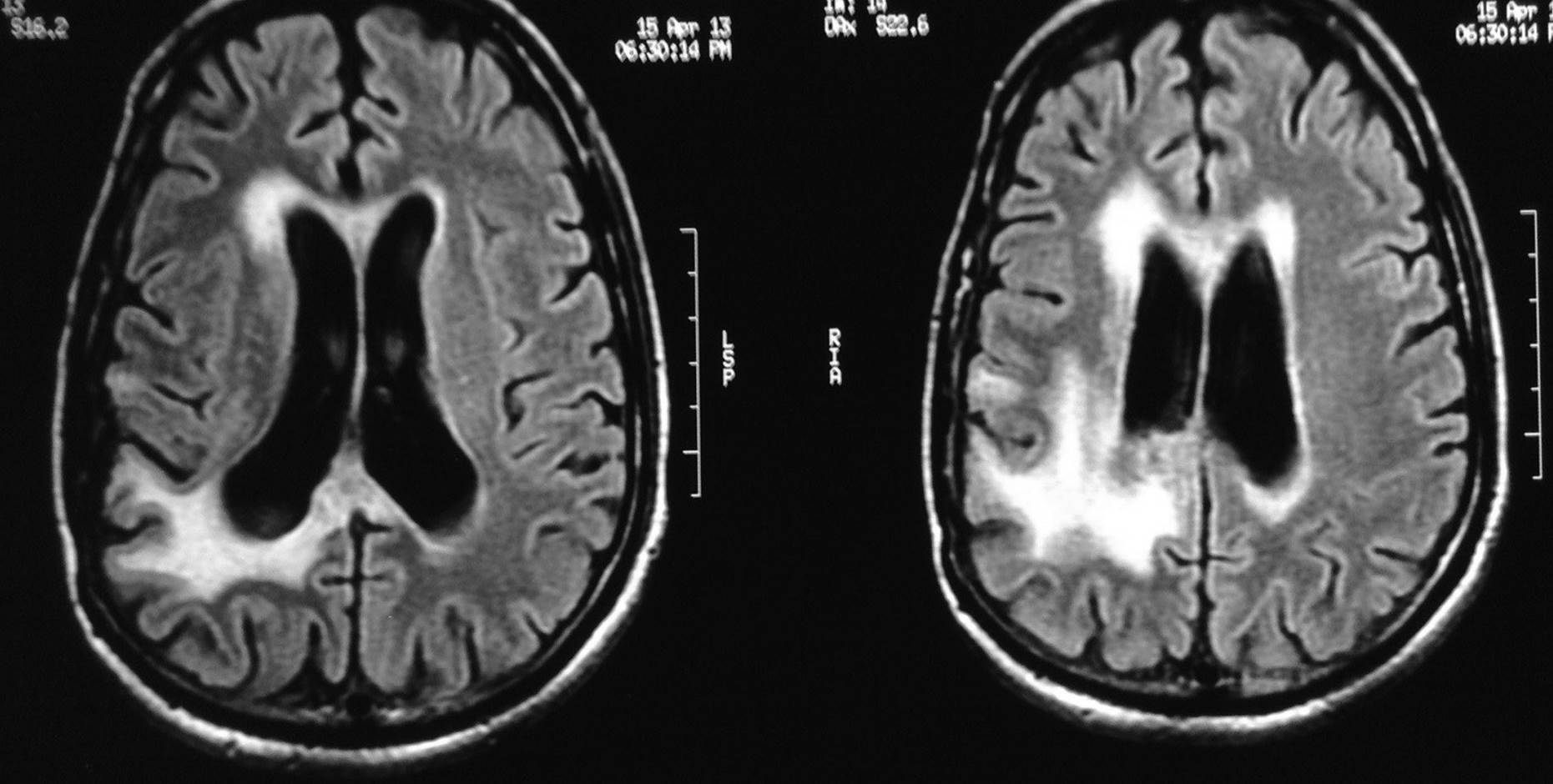
T2 Flair images
MRI scan 28.11.2011
Patient was planned for 6 adjuvant monthly cycles of Cap Temozolomide
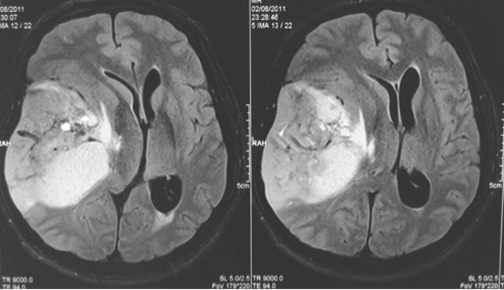
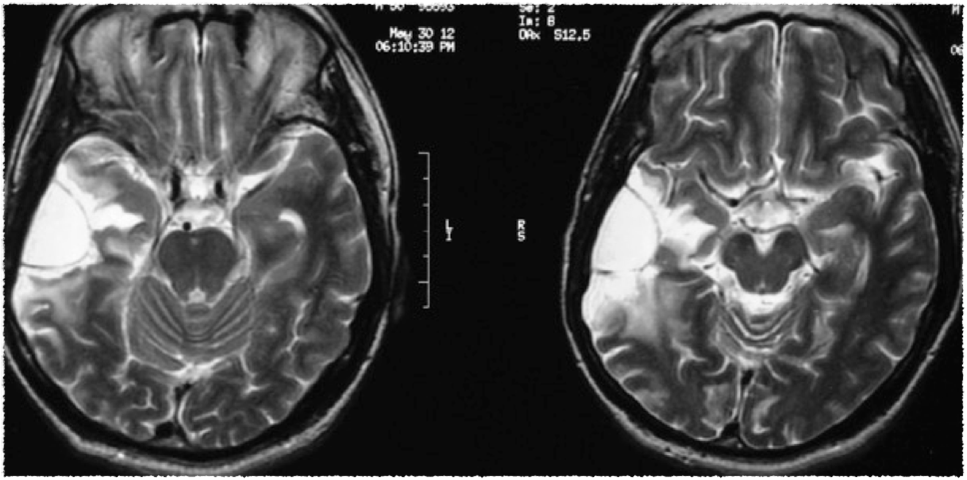
Follow up MRI scan was done after 6 cycles of adjuvant Temozolomide (completed in April 2012)
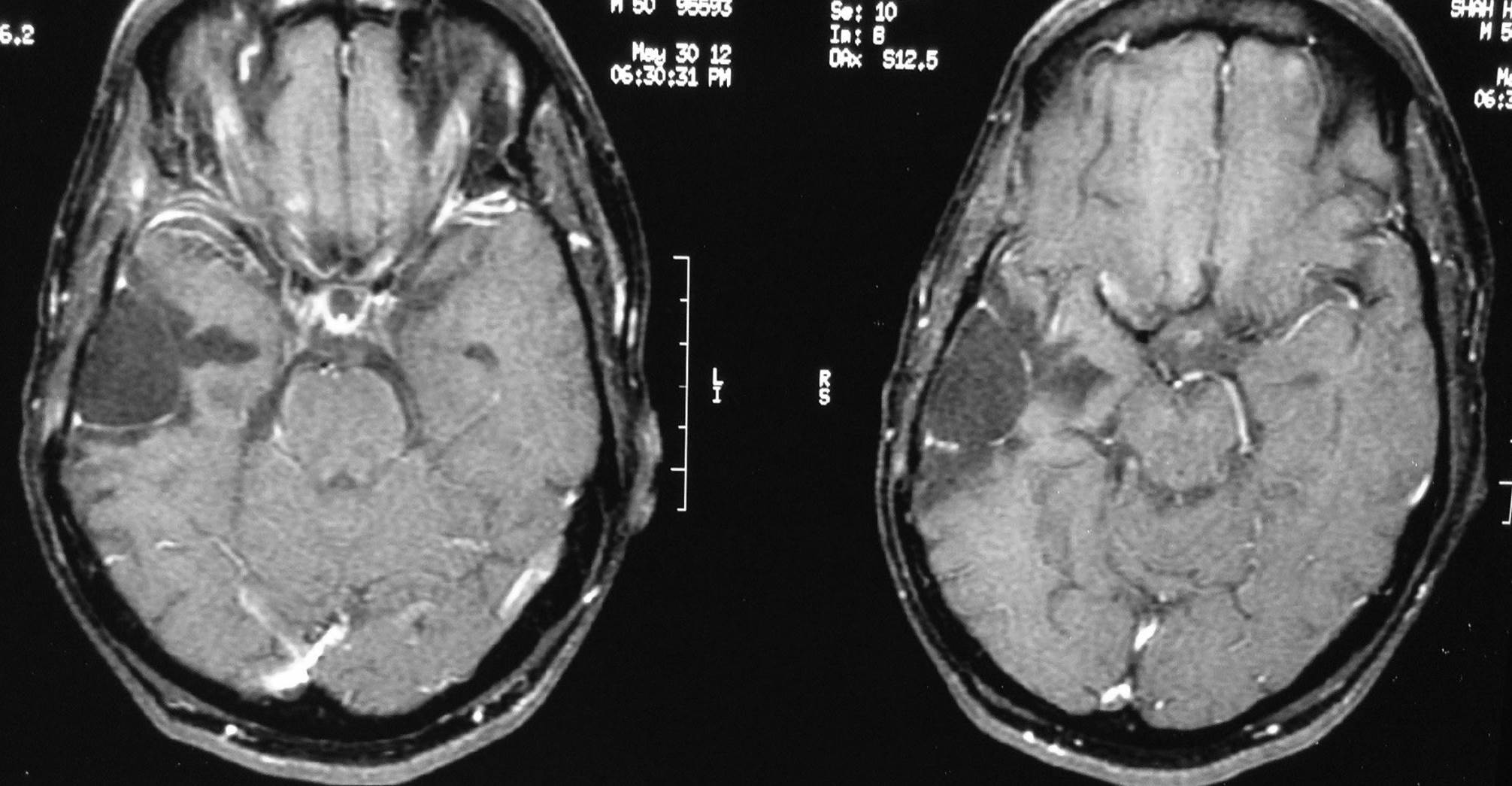
MRI scan done on 30.5.2012
T1 post contrast images Patient asymptomatic
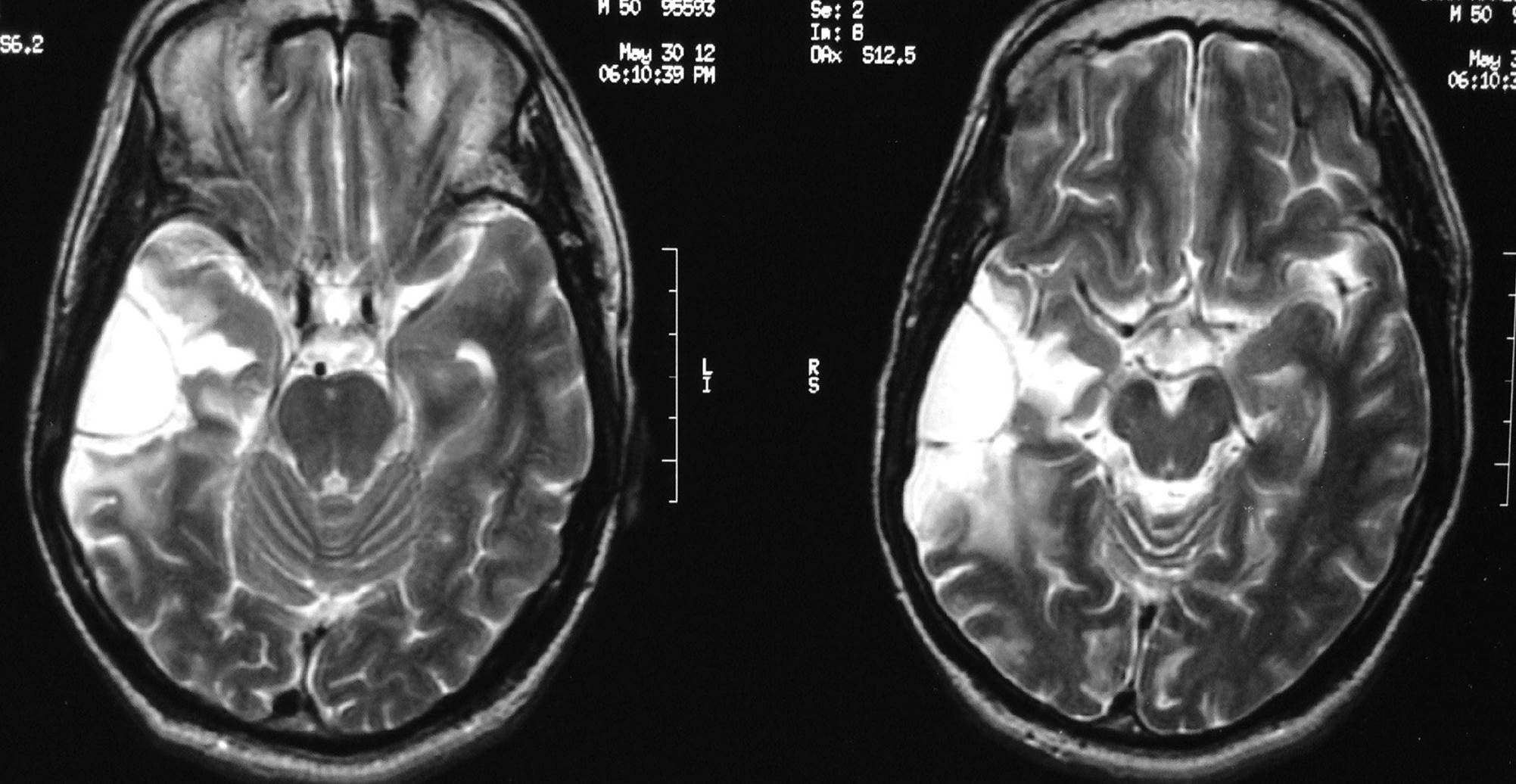
T2 Images
MRI scan 30.5.2012
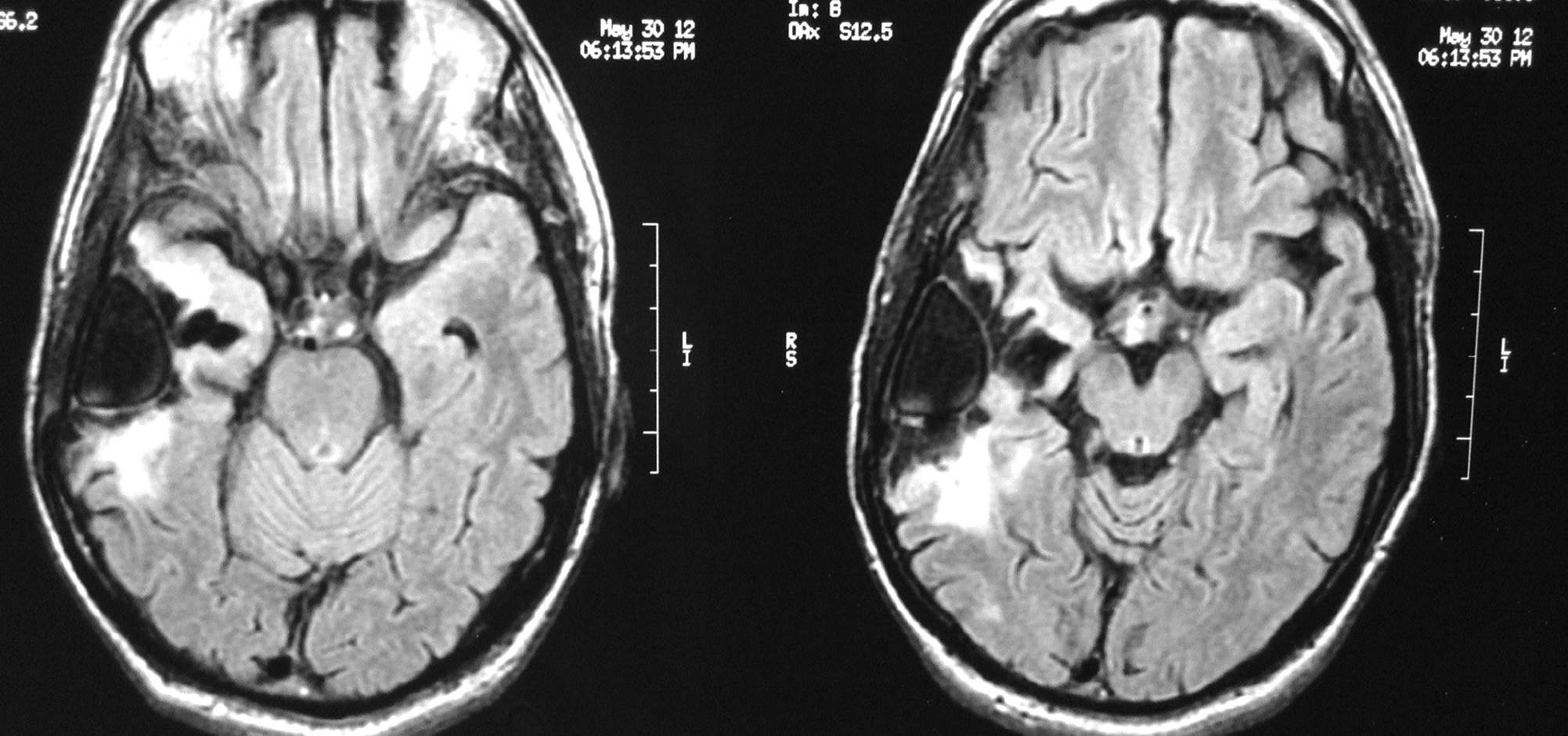
T2 Flair Images
MRI scan 30.5.2012
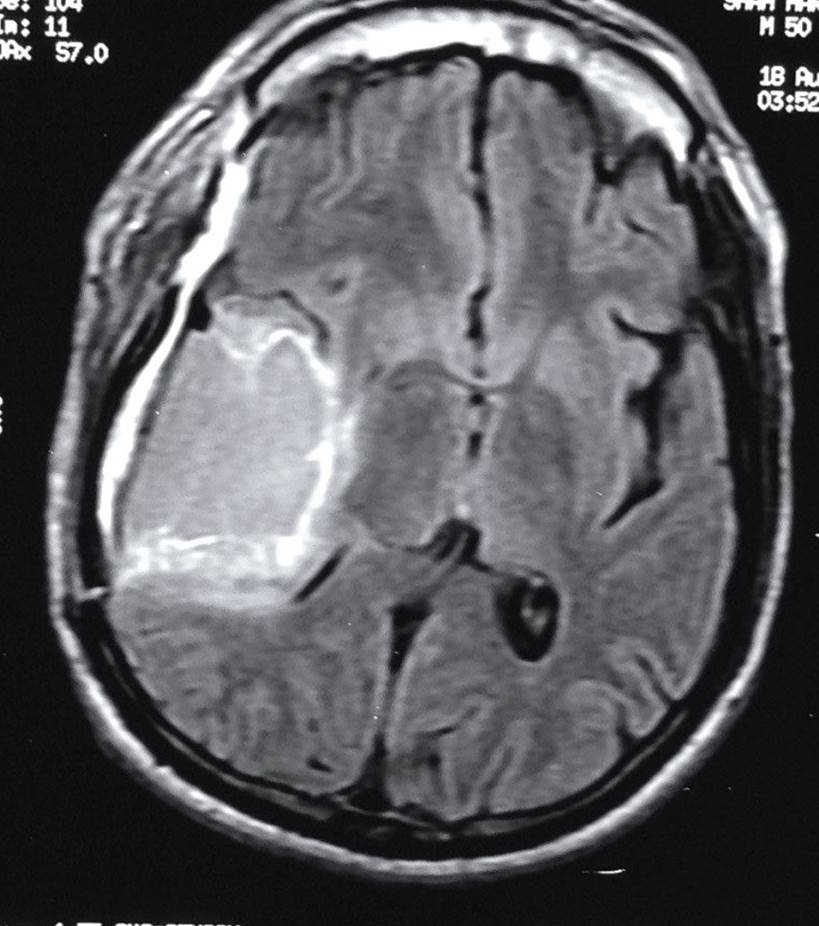
- He was kept on observation and was asymptomatic for over 9 months.
- He developed neurological symptoms (headache and gait disturbance) in February 2013.
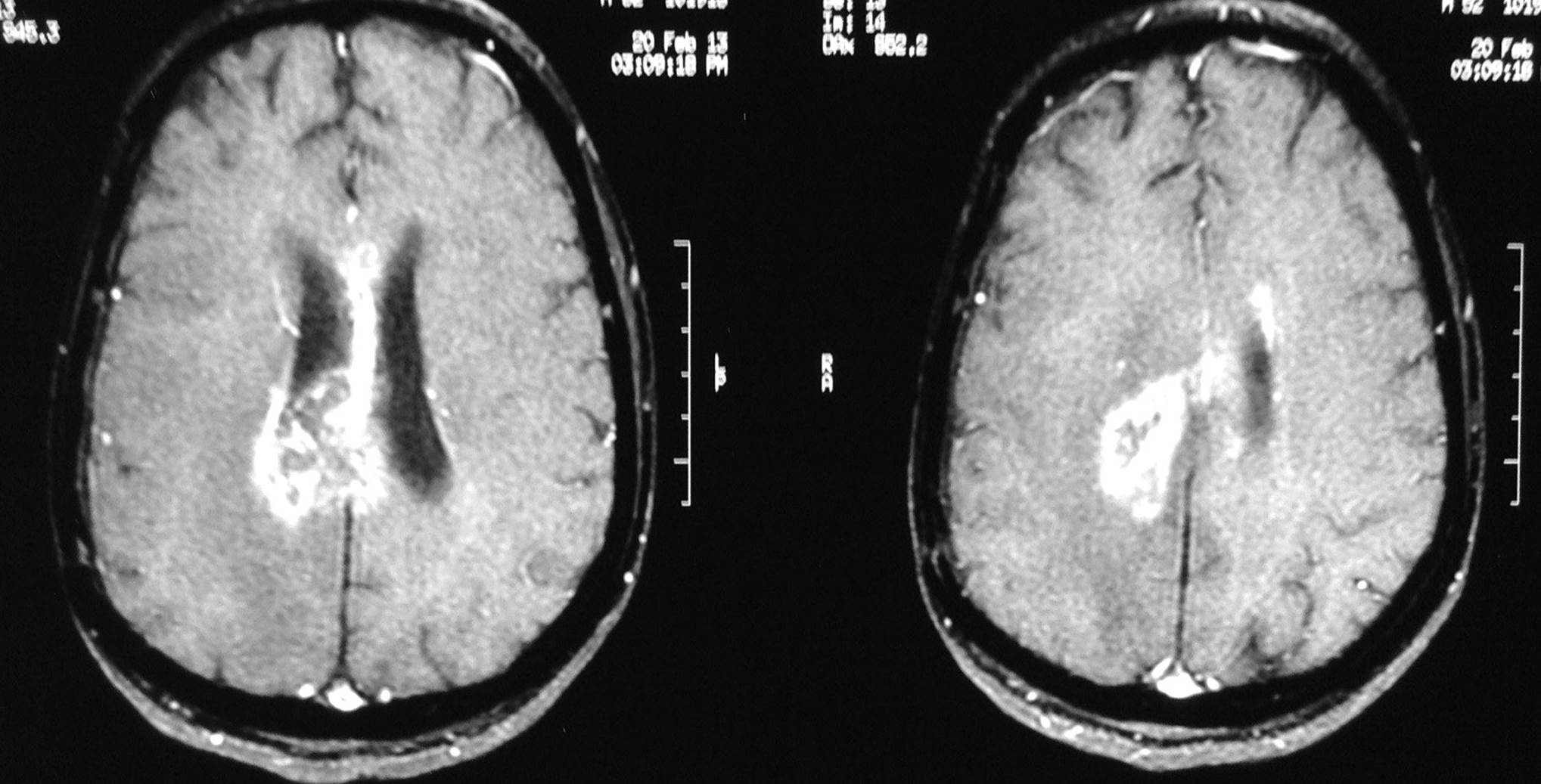
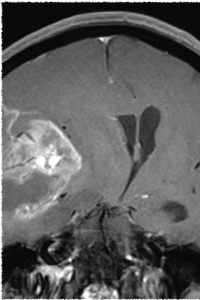
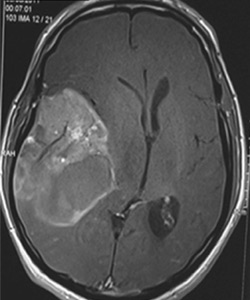
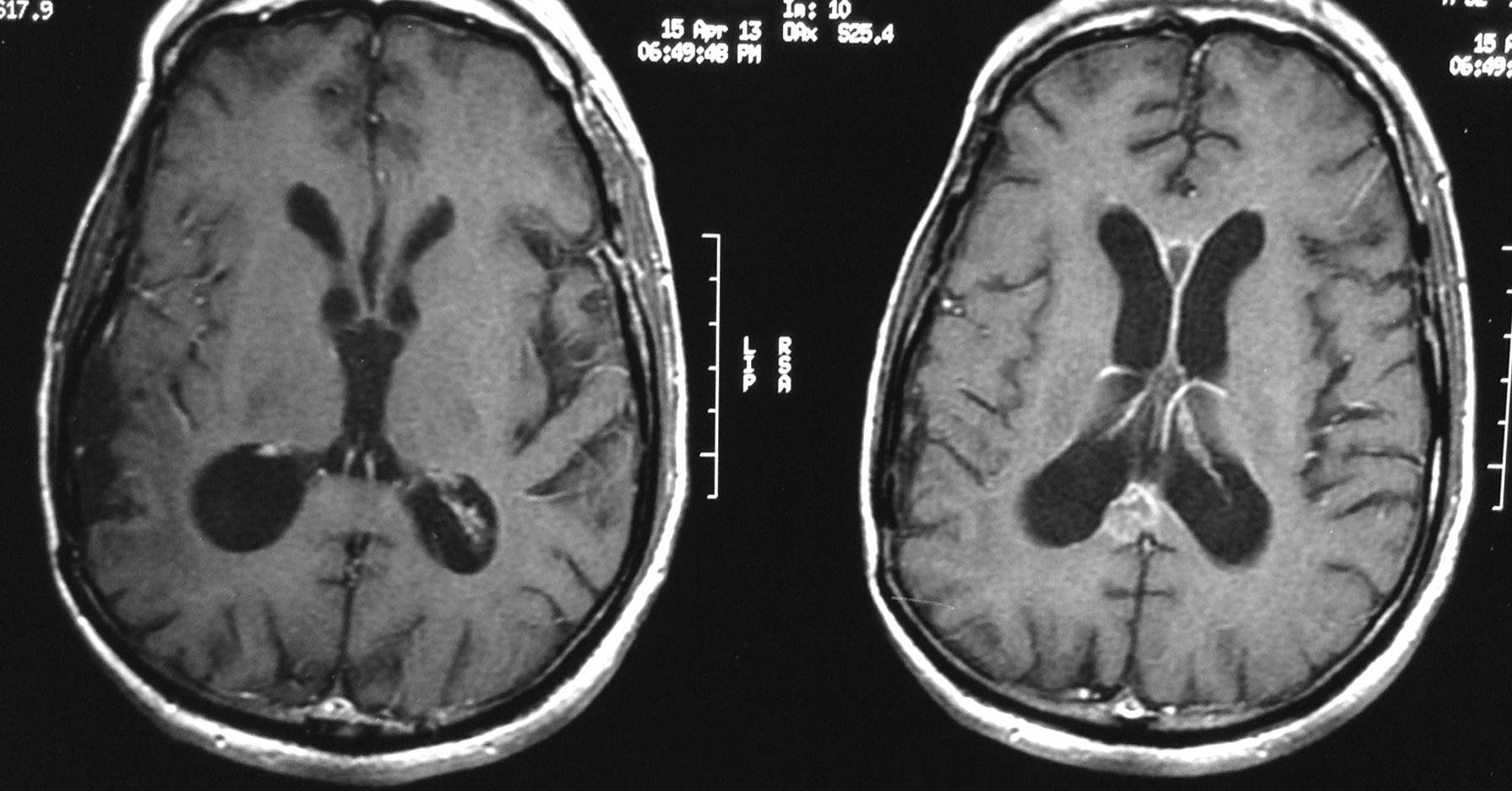
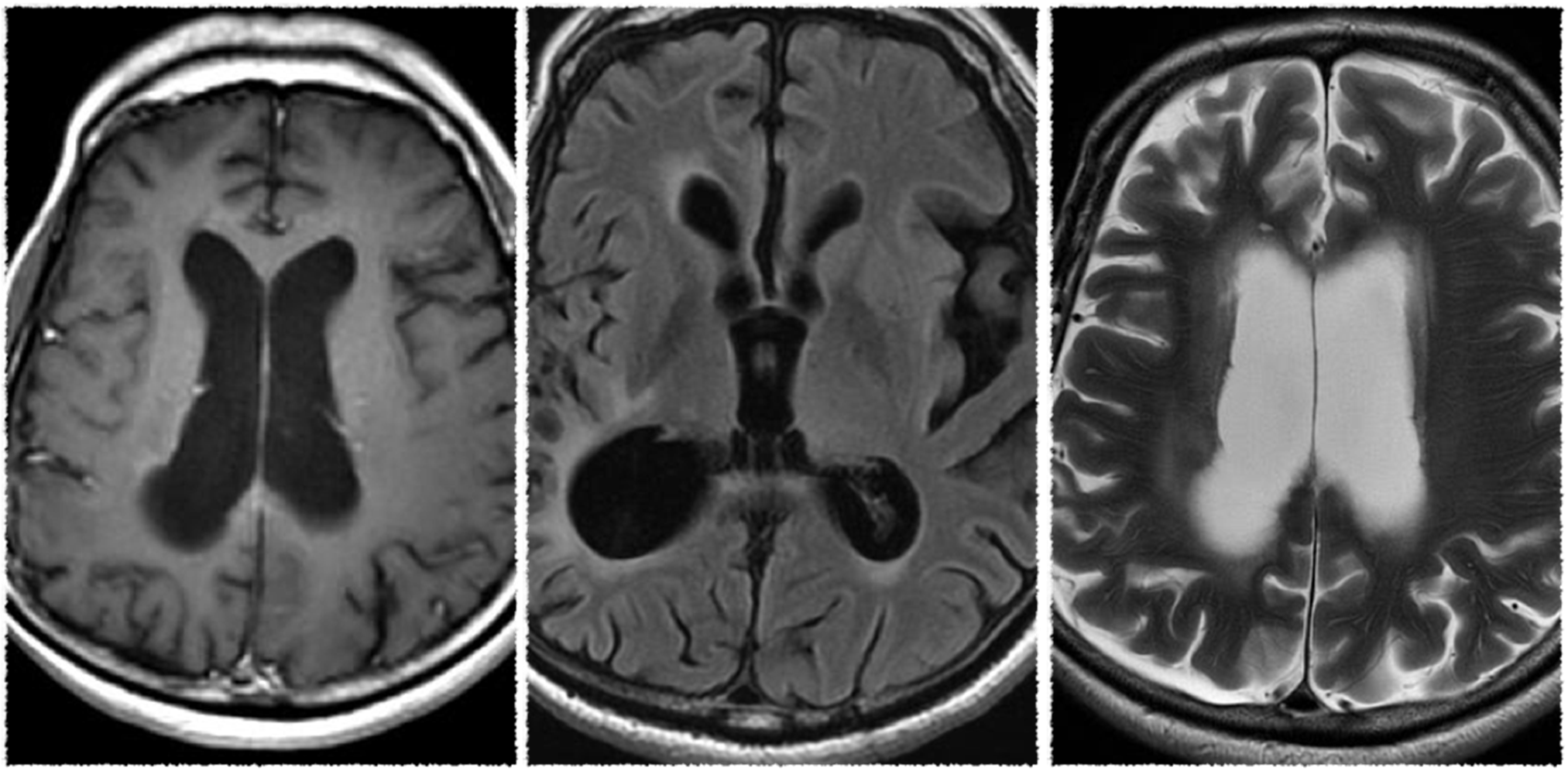
A MRI scan done on 20.2.2013
T1 post contrast images
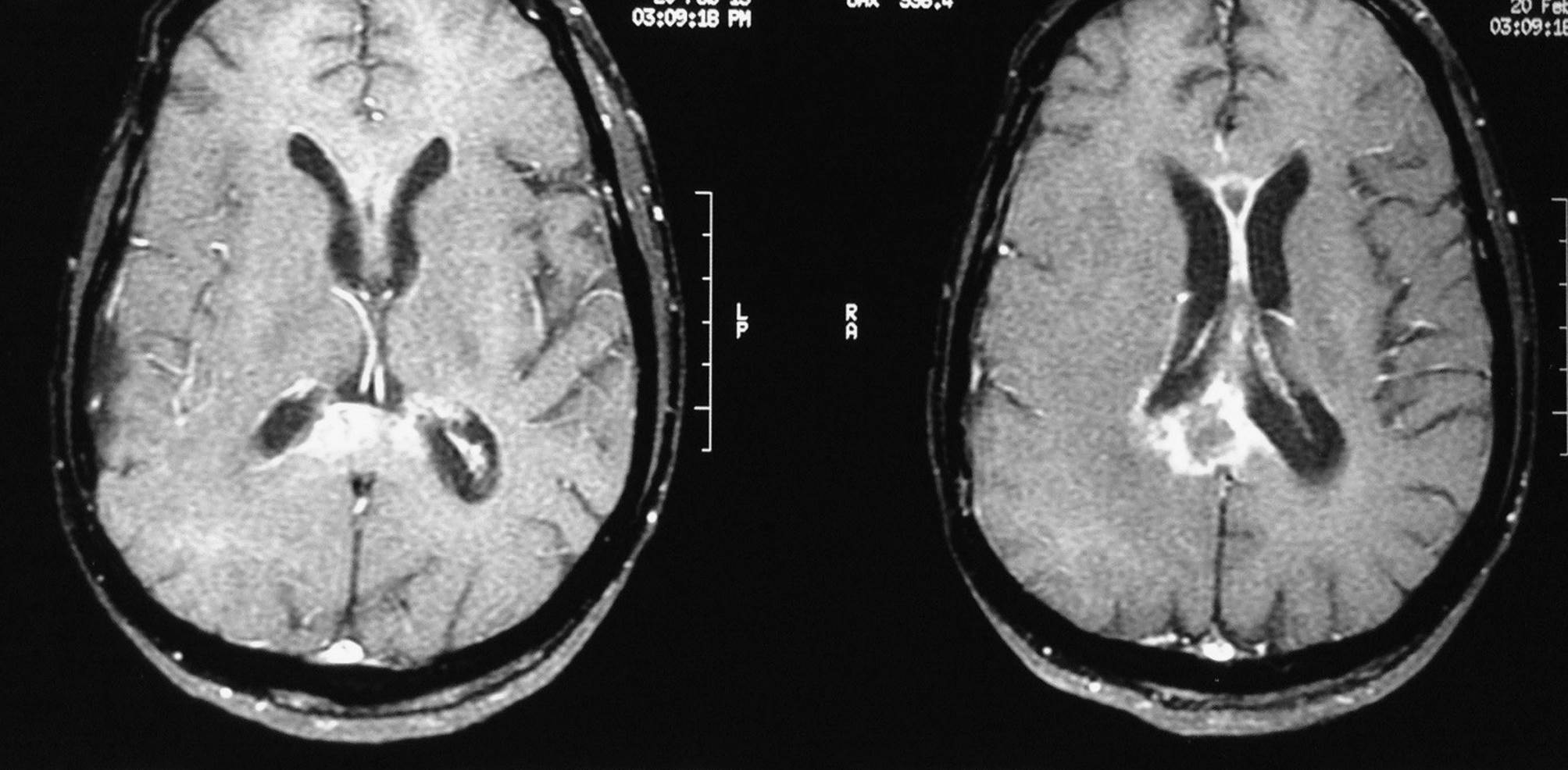
Coronal images
T2 FLAIR axial cuts
- What is the likely diagnosis?
- Is it tumour progression?
MR Spectroscopy revealed a tall lipid/lactate peak No significant choline peak identified
MR Spectroscopy revealed a tall lipid/lactate peak No significant choline peak identified
- Would steroids help?
- What is the quantum of benefit expected in steroid administration?
- Is complete clinical resolution expected to reflect on radiology as well?
After administration of steroids;
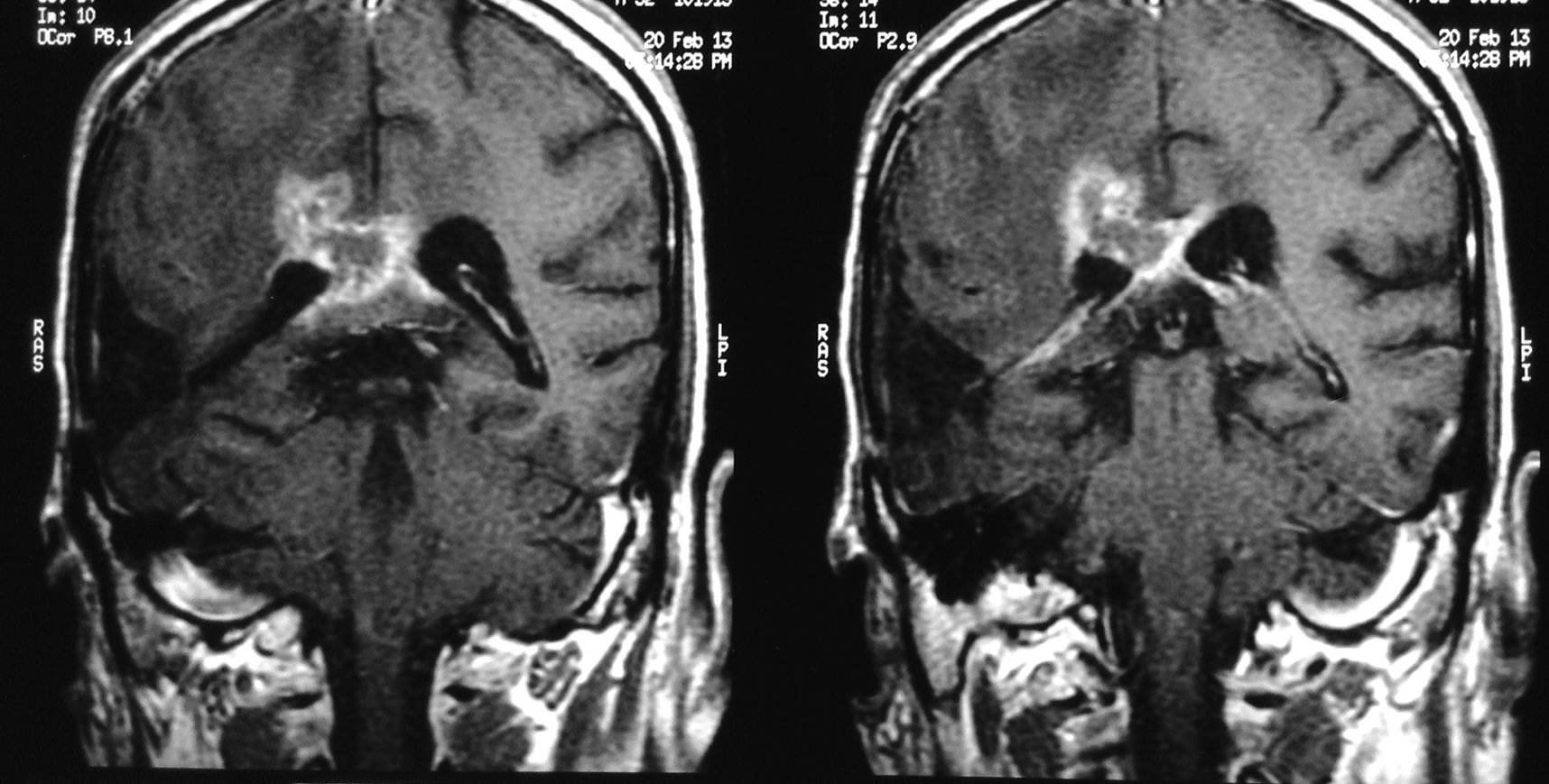
T1 Post Contrast axial cuts MRI scan done 2 months later, on 15.4.2013
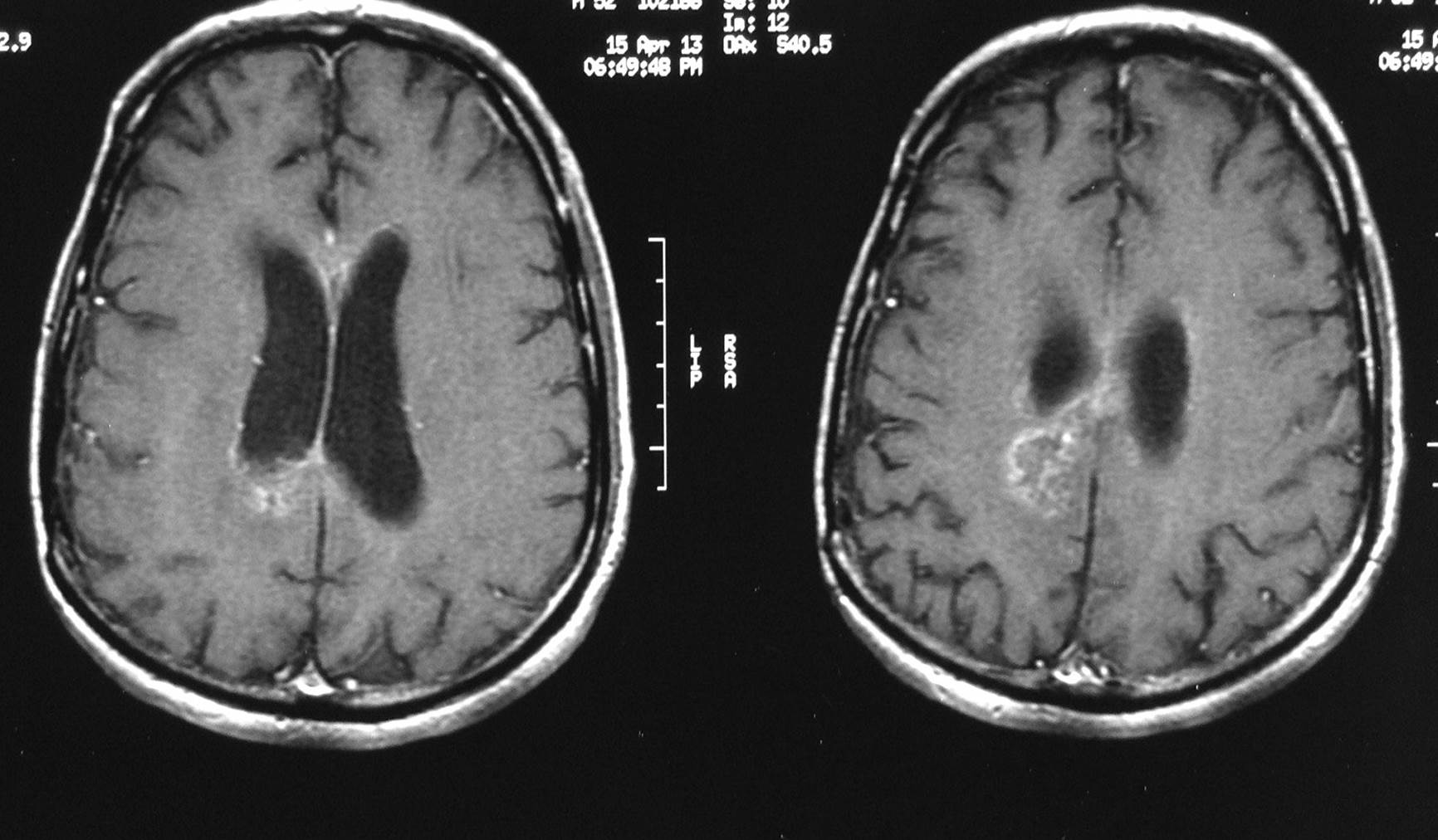
Significant resolution of the enhancing lesions
T2 images
T2 FLAIR axial cuts
Diagnosis: PSEUDOPROGRESSION
- Such changes have been described in early post RT+TMZ (typically within 3 months)
- These changes may however be seen even after several months on follow up (9 months in the presented case)
- The patient showed complete neurological recovery over several months with intermittent steroids and significant radiological resolution on MRI scans
MRI scan for follow up assessment was done in September 2014,
which shows excellent radiological response
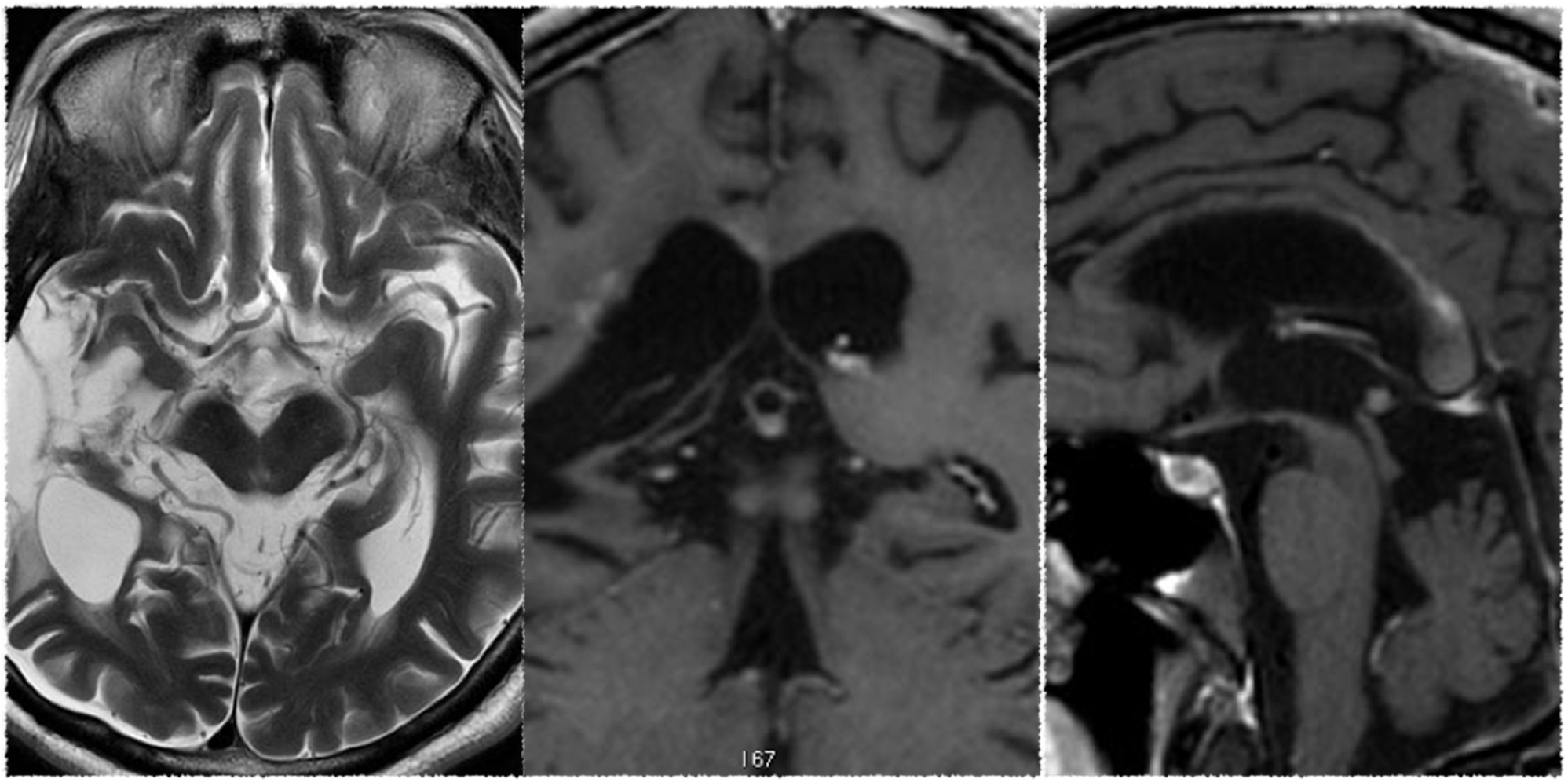
September 2014
Pseudoprogression
- Defined as the increase in the size of contrast-enhancing lesions; immediately after radiotherapy. Temozolomide accentuates the effect.
- Caused by vasodilation and disruption of blood brain barrier.
- Incidence of 25-40%
Differential Diagnosis
- Leukoencephalopathy syndrome
- True radio-necrosis
- Large vessel occlusion (Moya-Moya syndrome)
- Telengectasias
- White matter abnormalities
Management
- Close observation alone, if no or mild symptoms
- Steroids in tapering doses if symptomatic
- Recently anti-VEGF (Bevacizumab) has been tried with good success in refractory or steroid dependence.*
Message
- While a majority of patients will show these treatment related effects within few (1-3 months) after completing RT/RT+TMZ, these changes can be seen even several months after definitive treatment.
- Most patients show either no or mild symptoms but occasionally patients can be symptomatic too, especially if lesions are in eloquent area.
- To continue Temozolomide/observation even if apparent increase is seen on radiology.
- MR Spectroscopy and MR perfusion can aid considerably for confirmation and differentiating from true tumour progression (accuracy reported between 80-90%). Amino acid PET may help too.
- Cortex is invariably spared in these situations and any cortical involvement on MRI should raise a suspicion of true tumour progression.

